Type 2 Diabetes
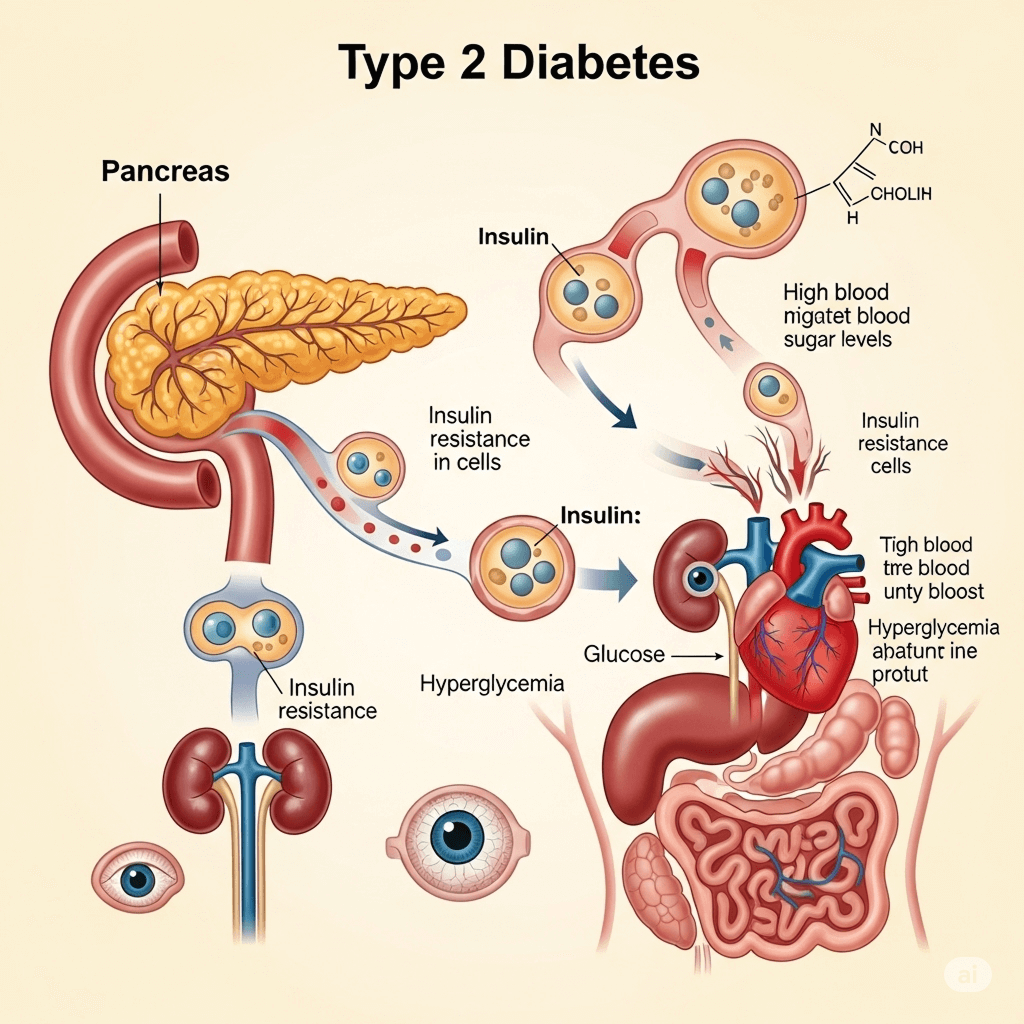
Type 2 Diabetes (T2D) is a chronic condition that affects how your body metabolizes sugar (glucose), which is your body's main source of fuel. It's the most common form of diabetes.
Without insulin, glucose builds up in the bloodstream, causing high blood sugar (hyperglycemia), which can lead to serious short- and long-term complications if not managed properly.
- Doesn't produce enough insulin: Insulin is a hormone made by the pancreas that acts like a key to let blood sugar into your cells for energy.
- Becomes resistant to insulin: Your cells don't respond well to insulin and don't take in enough sugar.
This leads to a buildup of glucose in your bloodstream, which can cause serious health problems over time if not managed.
Causes and Risk Factors
Type 2 Diabetes is often a combination of genetic and lifestyle factors. You're at higher risk if you
- Are overweight or obese: This is a primary risk factor, as excess weight can lead to insulin resistance.
- Are physically inactive: Lack of exercise contributes to insulin resistance.
- Have a family history of Type 2 Diabetes: Genetics play a significant role.
- Are older: The risk increases with age, especially after 45.
- Are of certain ethnic backgrounds: African Americans, Hispanic/Latino Americans, American Indians/Alaskan Natives, and Asian Americans are at higher risk.
- Have prediabetes: This means your blood sugar levels are higher than normal but not high enough to be diagnosed as diabetes yet. It's a strong warning sign.
- Have a history of gestational diabetes: Diabetes that develops during pregnancy.
- Have Polycystic Ovary Syndrome (PCOS): A common condition in women that can cause insulin resistance.
- Have high blood pressure or high cholesterol.
Symptoms
Many people with Type 2 Diabetes, especially in the early stages, have no symptoms or very mild ones. This is why many cases go undiagnosed for years. When symptoms do appear, they can include:
- Increased thirst and frequent urination
- Increased hunger
- Unintended weight loss
- Fatigue
- Blurred vision
- Slow-healing sores or frequent infections
- Numbness or tingling in the hands or feet
- Darkened areas of skin, usually in the armpits and neck (acanthosis nigricans)
Diagnosis
Type 2 Diabetes is diagnosed through blood tests that measure your blood glucose levels. Common tests include:
- A1C test: Measures your average blood sugar level over the past 2-3 months.
- Below 5.7% is normal.
- 5.7% to 6.4% indicates prediabetes.
- 6.5% or higher on two separate tests indicates diabetes.
- Fasting Plasma Glucose (FPG) test: Measures your blood sugar after an overnight fast.
- Below 100 mg/dL (5.6 mmol/L) is normal.
- 100 to 125 mg/dL (5.6 to 6.9 mmol/L) indicates prediabetes.
- 126 mg/dL (7.0 mmol/L) or higher on two separate tests indicates diabetes.
- Oral Glucose Tolerance Test (OGTT): Measures your blood sugar before and 2 hours after you drink a sugary liquid.
- Below 140 mg/dL (7.8 mmol/L) is normal.
- 140 to 199 mg/dL (7.8 to 11.0 mmol/L) indicates prediabetes.
- 200 mg/dL (11.1 mmol/L) or higher on two separate tests indicates diabetes.
- Random Plasma Glucose Test: A blood sugar test taken at any time.
- A level of 200 mg/dL (11.1 mmol/L) or higher, combined with symptoms, suggests diabetes.
Treament
The goal of Type 2 Diabetes management is to keep blood glucose levels within a target range to prevent complications. This usually involve:
- Healthy Eating: Focusing on whole, unprocessed foods, limiting sugar, refined carbohydrates, and unhealthy fats. Working with a registered dietitian is highly recommended.
- Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic activity per week, plus muscle-strengthening activities.
- Weight Management: Losing even a small amount of weight can significantly improve blood sugar control.
- Medications:
- Oral Medications: Many different types help in various ways (e.g., improve insulin sensitivity, reduce glucose production by the liver, stimulate insulin production). Metformin is often the first-line medication.
- Injectable Medications: Including GLP-1 receptor agonists (which help with weight loss and blood sugar) and, eventually, insulin if blood sugar targets aren't met with other treatments.
- Blood Sugar Monitoring: Regularly checking your blood glucose levels (with a glucometer or continuous glucose monitor - CGM) helps you and your healthcare team understand how food, exercise, and medication affect your levels.
- Stress Management: Stress can affect blood sugar.
- Regular Medical Check-ups: Seeing your doctor regularly for A1C tests, cholesterol checks, blood pressure monitoring, eye exams, foot exams, and kidney function tests.
In severe cases, it can lead to diabetic ketoacidosis (DKA) — a medical emergency where the body starts breaking down fat too quickly, leading to a buildup of acids (ketones) in the blood.
Long Term Complication(if not managed well)
Uncontrolled Type 2 Diabetes can lead to serious long-term complications:
- Cardiovascular disease: Heart attack, stroke, high blood pressure.
- Nerve damage (neuropathy): Tingling, numbness, pain, or weakness, especially in the feet.
- Kidney disease (nephropathy): Can lead to kidney failure requiring dialysis or transplant.
- Eye damage (retinopathy): Can lead to blindness.
- Foot damage: Poor blood flow and nerve damage increase the risk of infections and amputations.
- Skin conditions: Various skin issues can arise due to diabetes.
- Hearing impairment: Diabetes can increase the risk of hearing loss.
- Alzheimer's disease: Increased risk associated with diabetes.
Living with Type 2 Diabetes
While Type 2 Diabetes is a chronic condition, it can often be prevented, and in some cases, put into remission (blood sugar levels return to normal without medication) through significant lifestyle changes, especially if caught early (at the prediabetes stage).
- Weight loss: Even 5-7% of body weight can make a big difference.
- Healthy diet: Emphasize fruits, vegetables, whole grains, lean protein.
- Regular exercise: Stay active.
Donate
Your generous donations help us provide essential resources, fund groundbreaking research, and support programs that make a real difference in the lives of those affected by diabetes.
Volunteer
Join our volunteer team to make a difference in the lives of those affected by diabetes through community support and engagement.
Fundraise
Join us in raising funds to support diabetes research, education, and community programs, making a lasting impact together.
 Glucose Guardians
Glucose Guardians