Type 1 Diabetes
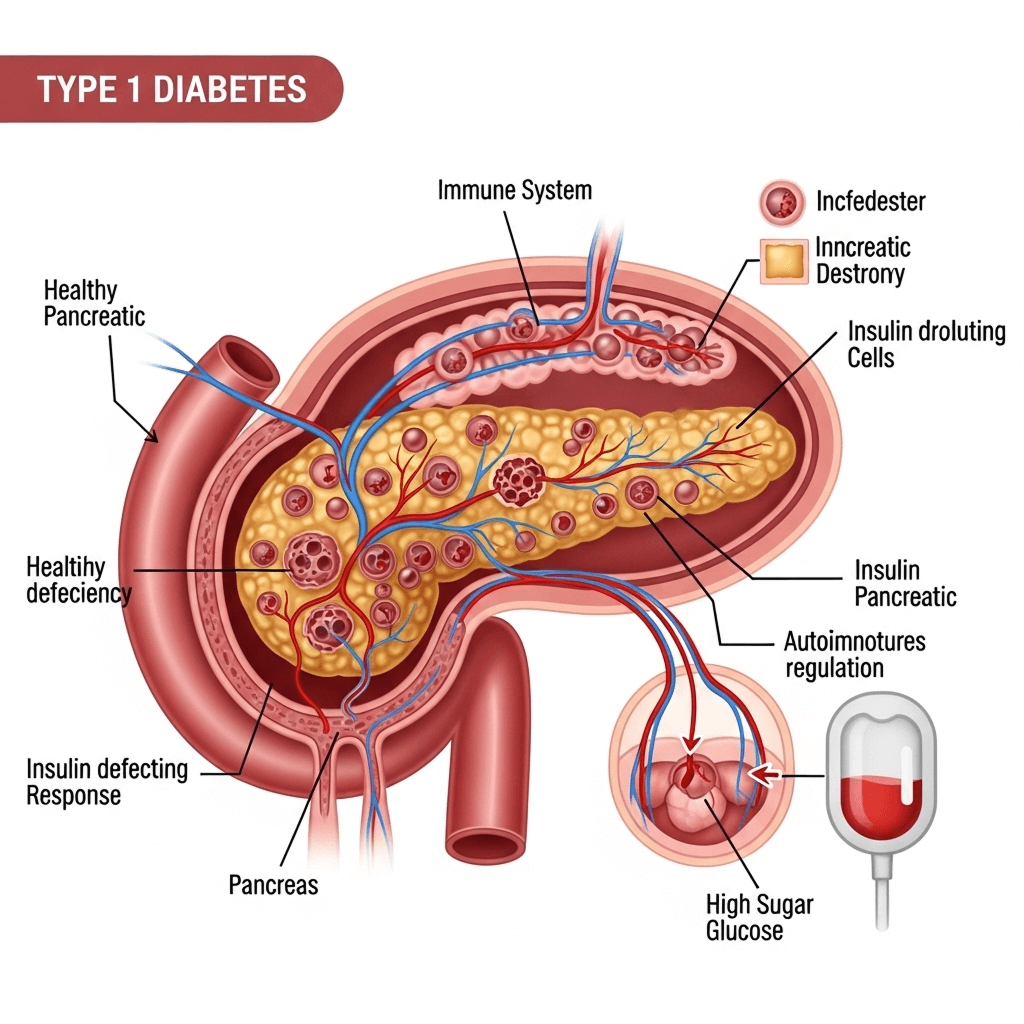
Type 1 Diabetes (T1D) is a chronic autoimmune condition in which the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Insulin is a hormone essential for allowing glucose (sugar) to enter cells and be used for energy.
Without insulin, glucose builds up in the bloodstream, causing high blood sugar (hyperglycemia), which can lead to serious short- and long-term complications if not managed properly.
Causes and Risk Factors
Causes (Suspected)
- Autoim mune response: The immune system targets pancreatic beta cells.
- Genetic predisposition: Certain genes (like HLA-DR3 and DR4) are linked to higher risk.
- Environmental triggers: Viral infections (e.g., enteroviruses, Coxsackie virus) might trigger the immune response.
- Family history: Having a sibling or parent with Type 1 increases risk.
Not Caused By
- Eating too much sugar
- Poor diet
- Lack of exercise
Who Gets It?
- Often diagnosed in children, adolescents, or young adults, which is why it’s also called juvenile diabetes.
- However, Type 1 can occur at any age.
- Affects about 5-10% of all people with diabetes.
Symptoms
Symptoms usually come on quickly, especially in children:
- Excessive thirst and dry mouth
- Frequent urination
- Extreme hunger (even while losing weight)
- Sudden weight loss
- Fatigue or weakness
- Blurred vision
- Irritability or mood changes
- Bed-wetting in children who previously didn’t
In severe cases, it can lead to diabetic ketoacidosis (DKA) — a medical emergency where the body starts breaking down fat too quickly, leading to a buildup of acids (ketones) in the blood.
Diagnosis
A healthcare provider will typically use the following tests:
- Fasting blood sugar
- Random blood glucose test
- HbA1c (glycated hemoglobin)
- Autoantibody tests (to distinguish Type 1 from Type 2)
- C-peptide test (measures how much insulin the body is producing)
Treatment
There is no cure for Type 1 Diabetes, but it is manageable. The key is daily insulin therapy and careful blood sugar management:
- Insulin Therapy
- Short-acting, long-acting, or intermediate-acting insulin
- Delivery via syringes, insulin pens, or insulin pumps
- Newer methods: automated insulin delivery systems (AID)
- Blood Glucose Monitoring
- Finger-prick tests or Continuous Glucose Monitors (CGMs)
- Diet and Nutrition
- Carbohydrate counting
- Balanced meals
- Avoid sugar spikes
- Excercise
- Helps with glucose control, but must be carefully balanced with insulin and food intake to avoid hypoglycemia (low blood sugar)
- Education and Support
- Diabetes self-management education (DSME)
- Support groups
- School nurse coordination
- Family counseling
Long Term Complication(if not managed well)
- Regular check-ups with healthcare providers
- Monitoring for complications (e.g., eye, kidney, nerve damage)
- Maintaining a healthy lifestyle
- Staying updated on new treatments and technologies
- Psychological support for mental health challenges
Living with Type 1 Diabetes
Living with T1D requires vigilance, but with the right support, people can live long, healthy, and active lives.
- Many athletes, celebrities, and professionals live with Type 1 successfully.
- Emotional and psychological support is crucial, especially for children and teens.
- Education is empowerment.
Donate
Your generous donations help us provide essential resources, fund groundbreaking research, and support programs that make a real difference in the lives of those affected by diabetes.
Volunteer
Join our volunteer team to make a difference in the lives of those affected by diabetes through community support and engagement.
Fundraise
Join us in raising funds to support diabetes research, education, and community programs, making a lasting impact together.
 Glucose Guardians
Glucose Guardians