Gestational Diabetes
Gestational Diabetes Mellitus (GDM) is a type of diabetes that develops or is first diagnosed during pregnancy. It's a significant health concern because it can affect both the pregnant person and the baby.
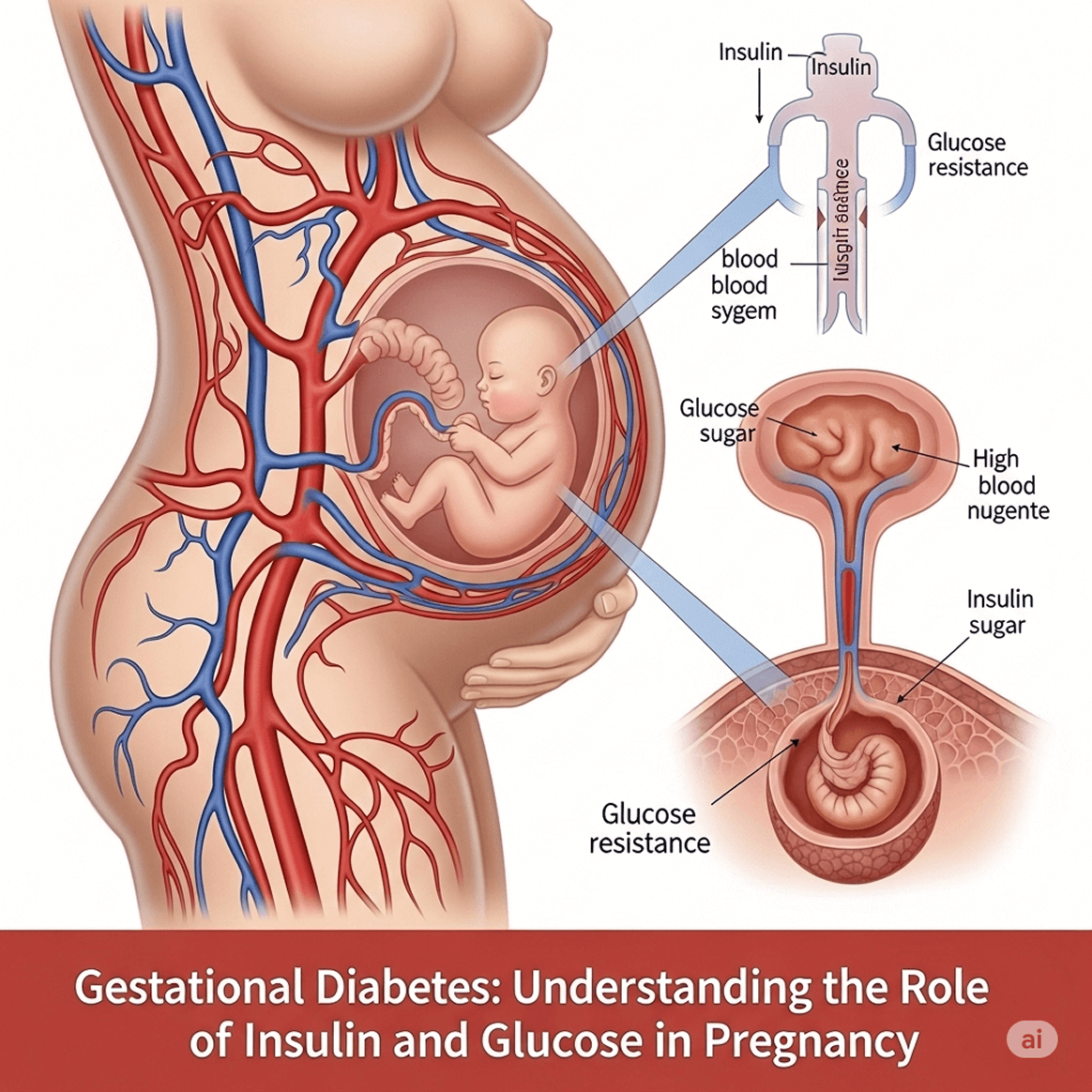
During pregnancy, the placenta produces hormones that help the baby grow. These hormones can make the body less responsive to insulin (known as insulin resistance). Normally, the pancreas responds by making more insulin to overcome this resistance. However, if the pancreas can't produce enough extra insulin to keep blood sugar levels normal, blood glucose levels rise, leading to GDM
Causes and Risk Factors
Causes (Suspected)
While the exact cause isn't always clear, GDM occurs when the body can't produce or effectively use all the insulin it needs during pregnancy. Several factors can increase a person's risk:
- Overweight or Obesity: Being overweight or obese before pregnancy or gaining too much weight during pregnancy.
- Lack of Physical Activity: Not being physically active.
- Prediabetes: Having blood sugar levels that are higher than normal but not high enough for a Type 2 diabetes diagnosis.
- Family History: A close relative (parent, sibling) with Type 2 diabetes.
- Previous Gestational Diabetes: Having GDM in a previous pregnancy.
- Previous Large Baby: Having given birth to a baby weighing more than 9 pounds (about 4 kg) in a previous pregnancy.
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder that can increase insulin resistance.
- Certain Ethnicities: Some ethnic groups have a higher risk, including African Americans, Hispanic/Latino Americans, American Indians/Alaskan Natives, and Asian Americans.
- Age: Being over 25 years old (risk increases with age).
Symptoms
Most people with GDM don't experience noticeable symptoms. When symptoms do occur, they are often mild and can be mistaken for normal pregnancy discomforts. These might include:
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
- Frequent infections (bladder, vaginal, skin)
Management and Treatment
The primary goal of GDM management is to keep blood sugar levels within a healthy range to prevent complications for both the pregnant person and the baby. Management typically involves:
- Healthy Eating Plan:
- Focus on balanced meals with appropriate portions of carbohydrates, proteins, and healthy fats.
- Spread carbohydrate intake throughout the day to avoid blood sugar spikes.
- Work with a registered dietitian specializing in prenatal nutrition.
- Regular Physical Activity:
- Engage in moderate-intensity exercise as approved by your doctor (e.g., brisk walking, swimming, prenatal yoga).
- Aim for at least 30 minutes on most days of the week.
- Blood Sugar Monitoring:
- You'll be taught how to check your blood sugar levels multiple times a day (e.g., fasting and after meals) using a blood glucose meter.
- This helps you and your healthcare provider understand how food, activity, and stress affect your levels.
- Medication (if lifestyle changes aren't enough):
- If diet and exercise aren't sufficient to control blood sugar, your doctor may prescribe medication.
- Insulin injections are the most common and safest medication during pregnancy, as insulin does not cross the placenta to the baby.
- Oral medications like Metformin or Glyburide might be considered in some cases, but insulin is generally preferred.
- Regular Medical Monitoring:
- Frequent prenatal appointments to monitor your blood sugar, the baby's growth, and overall health.
Screening and Diagnosis
GDM is typically diagnosed between 24 and 28 weeks of pregnancy, though it may be tested earlier if you have high-risk factors. The most common screening and diagnostic process involves:
- Glucose Challenge Test (GCT) / 1-Hour Glucose Test:
- You drink a sugary glucose solution.
- One hour later, your blood sugar is tested.
- If your blood sugar is above a certain threshold (e.g., 130-140 mg/dL or 7.2-7.8 mmol/L), you'll need a follow-up test. This is a screening, not a diagnosis.
- Oral Glucose Tolerance Test (OGTT) / 3-Hour Glucose Test (Diagnostic):
- You fast overnight.
- Your blood is drawn for a fasting blood sugar level.
- You drink a more concentrated sugary glucose solution.
- Your blood sugar is tested at 1, 2, and 3 hours after drinking the solution.
- If two or more of your blood sugar readings are above normal levels, you are diagnosed with GDM.
Post-Pregnancy Care
- Postpartum Glucose Test: Your blood sugar levels should be re-checked 6 to 12 weeks after delivery to ensure they have returned to normal.
- Ongoing Monitoring: Even if your blood sugar returns to normal, you remain at higher risk for developing Type 2 diabetes later in life. It's recommended to get tested for Type 2 diabetes every 1-3 years.
- Lifestyle Continuation: Continuing a healthy diet and regular exercise after pregnancy is crucial for reducing the risk of developing Type 2 diabetes.
- Breastfeeding: Breastfeeding can help both the baby and the parent. For the parent, it can help regulate blood sugar and reduce the risk of Type 2 diabetes.
Because symptoms are often absent or subtle, screening is crucial for all pregnant individuals.
Potential Risks and Complications
For the Baby
- Macrosomia (Large Baby): High blood sugar in the pregnant person can lead to the baby growing too large, increasing the risk of a difficult vaginal delivery, C-section, and birth injuries (e.g., shoulder dystocia).
- Hypoglycemia (Low Blood Sugar) at Birth: After birth, the baby's pancreas may continue to produce extra insulin, leading to low blood sugar shortly after delivery.
- Breathing Problems: Babies of mothers with GDM may be at higher risk for respiratory distress syndrome.
- Jaundice: Yellowing of the skin and eyes.
- Increased Risk of Obesity and Type 2 Diabetes Later in Life: Children born to mothers with GDM have a higher risk of developing obesity and Type 2 diabetes themselves.
For the Pregnant Person:
- Preeclampsia: A serious pregnancy complication characterized by high blood pressure and protein in the urine.
- Increased Risk of C-section: Due to larger baby size or other complications.
- Increased Risk of Developing Type 2 Diabetes Later: Approximately 50% of individuals who have GDM will develop Type 2 diabetes within 5 to 10 years after pregnancy. This risk is significant and requires ongoing monitoring.
- Future Gestational Diabetes: Higher chance of GDM in subsequent pregnancies.
Donate
Your generous donations help us provide essential resources, fund groundbreaking research, and support programs that make a real difference in the lives of those affected by diabetes.
Volunteer
Join our volunteer team to make a difference in the lives of those affected by diabetes through community support and engagement.
Fundraise
Join us in raising funds to support diabetes research, education, and community programs, making a lasting impact together.
 Glucose Guardians
Glucose Guardians